| Medically reviewed by
Robin Backlund, BHSc
Last update:

Preeclampsia is a significant health concern in pregnancy. It is defined by the American College of Cardiology as a hypertensive disorder occurring in 2-8% of pregnancies worldwide, leading to substantial morbidity and mortality.
This condition, which typically develops after 20 weeks of gestation, is characterized by new-onset hypertension and high levels of protein in the urine (proteinuria) and can impact various organs.
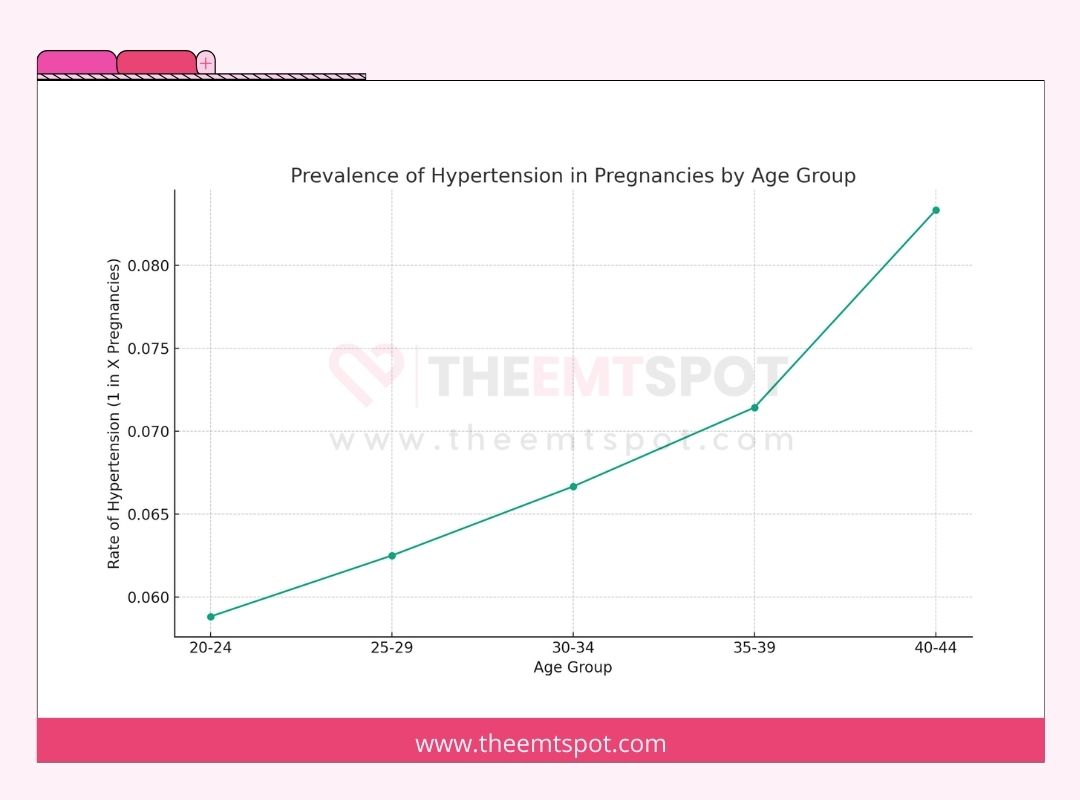
The Centers for Disease Control and Prevention (CDC) highlights that high blood pressure, or hypertension, is prevalent in the United States, occurring in 1 in every 12 to 17 pregnancies among women ages 20 to 44.
Apart from preeclampsia, other forms of high blood pressure during pregnancy include the following.
- Chronic hypertension, which is pre-existing high blood pressure before pregnancy
- Gestational hypertension is characterized by high blood pressure developing after 20 weeks without additional symptoms.
- Eclampsia is a severe progression of preeclampsia that involves seizures. Genetics and diet can increase your risk for eclampsia.
The difference between preeclampsia and eclampsia is critical. Preeclampsia involves high blood pressure and potential damage to organs, whereas eclampsia represents a more severe progression characterized by the onset of seizures, which can be life-threatening.
Preeclampsia is categorized into two types: mild and severe. While mild preeclampsia may have less severe symptoms and be managed with close monitoring, severe preeclampsia presents more serious symptoms and organ involvement, requiring immediate medical intervention.
The onset of preeclampsia typically occurs after the 20th week of pregnancy. However, it can begin earlier and is known to be a common condition, affecting about 1 in 25 pregnancies in the U.S..
A standard blood pressure chart during pregnancy shows varying normal ranges depending on the stage of pregnancy.
For instance, in the first trimester, the normal systolic blood pressure range is usually below 120 mmHg and diastolic below 80 mmHg. These ranges can slightly change as pregnancy progresses.
One main symptom of preeclampsia is high blood pressure. This is a critical sign for diagnosis and is typically accompanied by protein in the urine, although the latter might not always be present.
The primary cause and risk factor for preeclampsia is not fully understood, but it’s believed to be related to issues with the placenta.
Risk factors include a history of preeclampsia, first-time pregnancy, pre-existing conditions like hypertension or diabetes, obesity, and advanced maternal age. Genetic factors and immune system responses may also play a role.
Diagnosis typically involves checking blood pressure and assessing for signs like renal dysfunction.
The primary treatment method is delivery, especially in severe cases, with low-dose aspirin recommended for prevention in high-risk women.
One main danger of preeclampsia is the increased risk of cardiovascular and cerebrovascular complications, such as stroke or heart failure.
A significant prevention method involves lifestyle adjustments and possibly low-dose aspirin for those at high risk.
Contents
What are the types of preeclampsia?
Preeclampsia, a complication of pregnancy, manifests in two primary forms: mild and severe. Understanding these types is crucial for effective management and treatment.
Mild preeclampsia
- Mild preeclampsia is a less severe form of preeclampsia, a pregnancy-related condition characterized by elevated blood pressure and often accompanied by the presence of protein in the urine.
- In mild preeclampsia, symptoms are less pronounced and may include moderately elevated blood pressure levels and minimal proteinuria.
- This form typically allows for closer monitoring and the possibility of extending the pregnancy, delaying delivery to a safer time for the baby as long as the mother’s condition remains stable without signs of severe features or complications.
- According to a 2023 study published in Nature by researchers from the University of Melbourne, the risk of preeclampsia is higher in certain populations, such as Black women and women of South Asian origin.
Severe preeclampsia
- Severe preeclampsia is an advanced form of preeclampsia, a pregnancy complication characterized by significantly elevated blood pressure and often more pronounced protein in the urine.
- Unlike mild preeclampsia, severe preeclampsia presents with more intense symptoms and greater risks, necessitating closer medical monitoring and often earlier intervention, including potentially earlier delivery.
- A 2023 study from the University of Western Ontario identified a toxic protein, cis P-tau, as a central driver of preeclampsia.
- This breakthrough offers new insights into the cause and potential treatment for this condition, marking a significant advancement in understanding and managing severe preeclampsia.
What is the difference between mild and severe preeclampsia?
The transition from mild to severe preeclampsia can be rapid and is marked by an escalation in symptoms and organ damage.
While mild preeclampsia might be managed with close monitoring, severe preeclampsia often necessitates immediate medical intervention to manage the heightened risks to both mother and baby.
This distinction underscores the importance of vigilant health monitoring during pregnancy, especially for women with preeclampsia.
Aspect | Mild Preeclampsia | Severe Preeclampsia |
Blood Pressure | Elevated, but less than 160/110 mmHg | 160/110 mmHg or higher (Hypertensive emergency) |
Protein in urine | Present | Present, often in higher amounts |
Symptoms | Often no noticeable symptoms may include swelling of hands or face, weight gain | Severe headaches, changes in vision, light sensitivity, fatigue, nausea/vomiting, infrequent urination, abdominal and back pain |
Organ Involvement | Indicates potential kidney involvement | Significantly affects kidneys and liver; may cause fluid in the lungs, decreased platelet count |
Risk to mother and baby | Requires monitoring to prevent progression | Immediate medical attention is required due to high-risk |
Treatment | Regular monitoring may include medication to manage blood pressure | Hospitalization, medication for blood pressure and preventing seizures, potential early delivery |
What are the symptoms and signs of preeclampsia during pregnancy?
Preeclampsia during pregnancy manifests in varying degrees of severity, and understanding its symptoms is crucial for timely diagnosis and treatment.
The symptoms can be categorized into those associated with mild and severe preeclampsia, which is elaborated below.
Symptoms of mild preeclampsia
Mild preeclampsia may not present noticeable symptoms, making regular prenatal check-ups essential.
Dr. Christina Buchanan, an obstetrician with Providence St. Jude Medical Center, explains on verywellfamily.com.
“The first sign of preeclampsia may be elevated blood pressure at the doctor’s office along with protein in the urine.”
She further added that:
“Blood pressure greater than 140/90 and urine protein greater than or equal to 300 mg/24 hours can indicate mild preeclampsia.”
To summarize, symptoms of preeclampsia are added below.

- Moderately elevated blood pressure levels
- Minimal proteinuria (protein in the urine)
- Possible swelling in the hands and feet
- Mild headache
- Occasional vision changes, like blurriness or light sensitivity
- Slight upper abdominal discomfort
Symptoms of severe preeclampsia
Severe preeclampsia presents more significant symptoms; however, these symptoms often become noticeable after some damage has already occurred.
According to Dr. Sherry Ross from Providence Saint John’s Health Center:
“When a pregnant person’s blood pressure is greater than 160/110 and urine proteinuria measures at 3+ or higher on a urine dipstick, a diagnosis of severe preeclampsia may be made.”
She also emphasized that:
‘Severe preeclampsia can lead to maternal seizures, placental abruption, and fetal and maternal death, so early diagnosis and intervention are a matter of life and death.”
Despite its risky nature, a few symptoms as mentioned below, can help with early diagnosis and effective treatment.
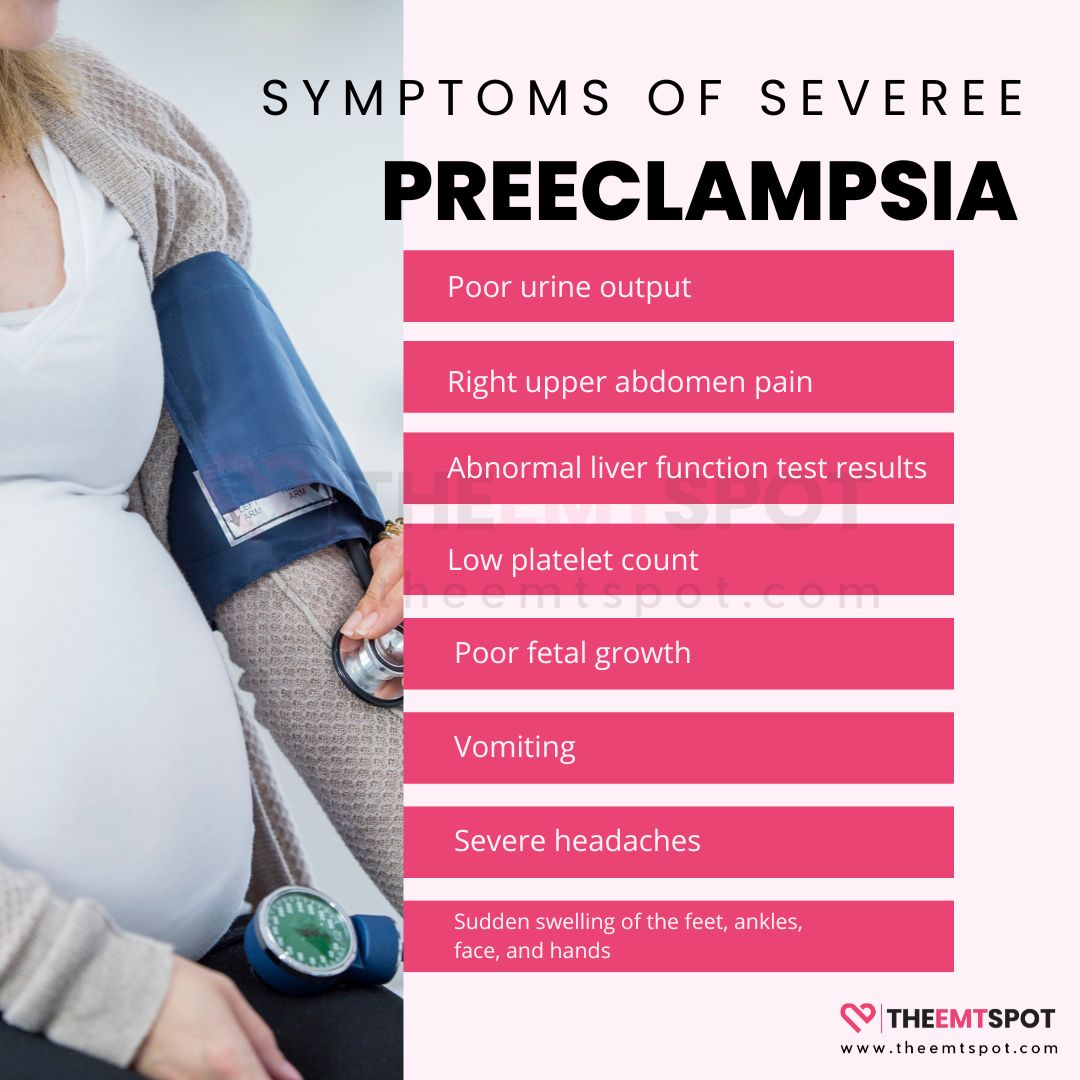
- Poor urine output
- Right upper abdomen pain
- Abnormal liver function test results
- Low platelet count
- Poor fetal growth
- Vomiting
- Severe headaches
- Sudden swelling of the feet, ankles, face, and hands.
What are the causes and risk factors of preeclampsia?
The causes and risk factors of preeclampsia are multifaceted, with several conditions and circumstances increasing the likelihood of its development during pregnancy.
Mayo Clinic has conducted a comprehensive review of the causes and risk factors. According to their findings, below are some of the factors to watch out for if you’re pregnant.
- Preeclampsia in a previous pregnancy: Women who have experienced preeclampsia in past pregnancies are at a higher risk.
- Multiple gestation: Having more than one baby (such as twins or triplets) increases the risk.
- Chronic high blood pressure: Women with a history of hypertension before pregnancy are more susceptible.
- Diabetes: A person with pre-existing diabetes has an increased risk of preeclampsia.
- Kidney disease: Pre-existing kidney disease can elevate the risk of developing preeclampsia.
- Autoimmune disorders: Conditions like lupus can increase the likelihood of preeclampsia.
- Use of in-vitro fertilization: Women who conceive through IVF may have an increased risk.
One of the major risk factors is the inconsistency in national guidelines for fetal surveillance in preeclamptic pregnancies.
A 2019 study published by Prof. Racheal Fox and her group in the Journal of Clinical Medicine, in fact, highlights this disparity and demands an evidence-based approach to figure out the right ways, timing, and how often we should evaluate this disease.
Does stress cause preeclampsia?
According to current medical understanding and research, stress does not directly cause preeclampsia.
However, stress may lead to high blood pressure during pregnancy, which increases the risk of serious conditions such as preeclampsia, preterm birth, and having a low-birthweight infant.
A study detailed in the journal Obstetrical and Gynecological Survey explored the relationship between psychological stress and preeclampsia.
The findings suggest that while stress is a factor in overall health, especially during pregnancy, it is not a direct cause of preeclampsia.
Preeclampsia is believed to result from a combination of genetic, nutritional, and environmental factors, with abnormal placental development playing a significant role.
Can you have preeclampsia without high blood pressure?
Preeclampsia is typically characterized by high blood pressure, but there are instances where it can occur without this classic symptom.
Some health institutions note that pregnant women, even those without a history of high blood pressure, can develop preeclampsia and may not exhibit the more obvious symptoms associated with the condition.
This fact underscores the importance of early detection, as the absence of high blood pressure does not necessarily rule out preeclampsia.
The 2017 case report ‘Atypical preeclampsia – Gestational proteinuria,’ in the Journal of Family Medicine and Primary Care, presents an unusual case of preeclampsia without high blood pressure, emphasizing the importance of recognizing atypical symptoms in preeclampsia management.
This case suggests the possibility of atypical presentations of preeclampsia, where hypertension is not a presenting feature.
However, it is important to note that such instances are relatively rare, and more research is needed to fully understand how preeclampsia can develop in the absence of high blood pressure.
How is preeclampsia diagnosed?
Diagnosing preeclampsia involves a combination of regular health checks and specific tests.
During prenatal visits, the doctor monitors a pregnant woman’s blood pressure, with readings of 140/90 mmHg or higher after the 20th week of pregnancy, indicating a potential concern.
The diagnostic process adheres to the criteria set by the American College of Obstetricians and Gynecologists (ACOG), outlined as follows.
- High blood pressure: When a blood pressure reading of 140/90 mmHg or higher is recorded twice, with at least 4 hours between readings, in a woman who previously had normal blood pressure before the 20th week of pregnancy.
- Proteinuria: Presence of protein in the urine, confirmed through a urine test.
- Other organ dysfunction (if proteinuria is absent): Signs of kidney or liver involvement, neurological symptoms, or hematological changes can also indicate preeclampsia.
- Blood clot abnormalities: Abnormalities in the body’s blood clotting mechanisms leading to increased or decreased clot formation indicate preeclampsia.
- Ultrasound scan: Ultrasound imaging of the baby can provide non-invasive diagnostic information about abnormalities in the baby’s growth.
- Physical examination: Fetal heart rate checks and physical exams for swelling or abdominal tenderness are crucial in diagnosing preeclampsia.
This multifaceted approach ensures a thorough evaluation, which is critical for the health and safety of both the mother and the baby.
What are the treatment methods for preeclampsia?
The treatment for preeclampsia largely depends on the stage of pregnancy and the severity of the condition. The primary objective is to manage the health of both the mother and the fetus while mitigating risks.
According to The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NIHCHD), if the pregnancy has reached 37 weeks or more, the healthcare provider typically delivers the baby to address preeclampsia and prevent additional issues.
However, if the pregnancy is under 37 weeks, they may explore treatment choices that allow the baby more time to mature, depending on the severity of the condition.
The guidelines set by NIHCHD and various other health institutions like the Mayo Clinic and Cleveland Clinic recommend the following treatment protocol.
- Diagnosis and treatment initiation: Once diagnosed with preeclampsia, the patient is closely monitored and referred to a specialist for further evaluation and care. This may involve regular follow-up or hospitalization for more intensive monitoring.
- Management based on gestational age: Management strategies vary with gestational age and the severity of preeclampsia. Beyond 37 weeks, delivery is typically initiated to resolve the condition.
- Preterm preeclampsia: If preeclampsia occurs before term without severe features, delivery may be delayed until 37 weeks for fetal growth. Severe features may necessitate earlier delivery to prevent complications.
- Maternal and fetal monitoring: During delayed delivery, close monitoring includes frequent blood pressure checks, liver and kidney function tests, and platelet counts for the mother. Fetal monitoring involves nonstress tests and ultrasound exams.
- Medication use: Medications can lower blood pressure and reduce stroke risk in the mother but don’t address underlying placental issues or prevent disease progression.
- Vaginal vs. cesarean delivery: The delivery method depends on factors like fetal position, cervical status, and overall fetal condition. In most cases, vaginal delivery is possible.
- Steroid administration: Steroids like betamethasone are given for likely preterm births (before 34 weeks) to enhance fetal lung development and reduce preterm birth complications.
What are the best medications for preeclampsia?
The primary focus of medications used to treat preeclampsia is symptom management, particularly addressing high blood pressure and preventing complications.
In emergency situations involving preeclampsia, commonly employed medications include intravenous (IV) hydralazine, labetalol, and oral nifedipine.
These drugs are effective at swiftly reducing elevated blood pressure levels and are typically administered in a hospital setting with close supervision.
An article in the journal Drugs, authored by Catherine M. Brown and Vesna D. Garovic, highlights the major medications used in women diagnosed with preeclampsia.
They recommend methyldopa and labetalol as suitable first-line options for controlling high blood pressure in cases of preeclampsia.
Methyldopa has a long history of use due to its safety profile during pregnancy, while labetalol is favored for its ability to manage blood pressure effectively without significantly impacting the fetal heart rate.
It’s essential to be aware that certain medications are not recommended for managing preeclampsia.
Specifically, beta-blockers and angiotensin-converting enzyme (ACE) inhibitors are generally avoided due to their potential adverse effects on the developing fetus.
Is there a cure for preeclampsia?
Currently, there is no definitive cure for preeclampsia, and the most effective treatment often involves delivering the baby, which can resolve the condition.
However, the decision to deliver depends on the stage of pregnancy and the severity of the condition.
According to the practice bulletin titled “Gestational Hypertension and Preeclampsia” by the ACOG, managing the condition is considered best practice.
When it’s too early for safe delivery, the focus shifts to prolonging the pregnancy as long as it’s safe for both the mother and the baby.
This management approach may include close monitoring, medication to control blood pressure, and sometimes hospitalization.
Further research is needed to elucidate the root cause of this disease and gain a better understanding of the underlying causes of preeclampsia.
What are the most common complications of preeclampsia?
Preeclampsia can lead to several complications, some of which are life-threatening.
These complications arise due to the impact of high blood pressure on various organs and systems in the body.
Ian Wilkinson, a clinical pharmacologist and professor of therapeutics at Cambridge University, highlights the gravity of these complications in The Guardian.
“The two major complications in preeclampsia are stroke and prolonged fitting,” he explains.
He added:
“In preeclampsia, elevated blood pressure and leaky capillaries can cause a bleed in the brain, leading to a stroke. Additionally, inflammation in the brain can trigger seizures (fitting).”
Wilkinson notes that complications often become fatal when symptoms like severe headaches are not recognized as signs of emergency or when monitoring is not as thorough as required.
The most common complications of preeclampsia are listed below.
- Stroke: Due to high blood pressure and leaky capillaries leading to bleeding in the brain.
- Seizures (eclampsia): Caused by inflammation in the brain.
- HELLP syndrome: An advanced stage of preeclampsia impacting both the liver and blood.
- Organ damage: Particularly to the kidneys, liver, and brain, due to elevated blood pressure.
- Fetal complications: Including growth restriction, premature birth, and low birth weight.
- Placental abruption: When the placenta separates from the uterus prematurely, resulting in bleeding.
- Cardiovascular issues: Preeclampsia increases the risk of future heart disease.
How does preeclampsia affect the mother?
Preeclampsia significantly affects maternal health. According to a report published in BMC Pregnancy and Childbirth, it is a leading cause of maternal deaths worldwide, with higher mortality rates in pregnancies complicated by preeclampsia compared to non-preeclamptic ones.
The condition has a multifactorial origin, influenced by factors such as maternal age, pre-existing medical conditions like chronic hypertension and diabetes, obesity, and certain genetic and environmental factors.
According to NICHD, preeclampsia impacts the following aspects of maternal health.
- High blood pressure: The hallmark symptom can lead to serious cardiovascular complications.
- Organ damage: Particularly affecting the kidneys, liver, and brain, potentially leading to long-term health issues.
- Severe complications: Including eclampsia (seizures), stroke, and HELLP syndrome (hemolysis, elevated liver enzymes, low platelet count).
- Impact on future health: Women with a history of preeclampsia have a higher risk of cardiovascular diseases later in life.
- Overall health impact: Poses a significant long-term threat to maternal health due to the damage caused by high blood pressure.
How does preeclampsia affect the baby?
Preeclampsia can significantly impact the baby during pregnancy, leading to various complications.
According to NICHD, preeclampsia can cause problems with the placenta early in pregnancy, resulting in several effects on the fetus. The following outlines more of its impact on the baby.
- Insufficient oxygen and nutrients lead to impaired fetal growth.
- An increased risk of preterm birth.
- The potential for stillbirth, particularly in cases of placental abruption.
- The possibility of infant mortality in severe cases.
- Long-term health issues for infants born prematurely, including learning disorders, cerebral palsy, epilepsy, deafness, and blindness.
- Additionally, infants who experience inadequate growth in the uterus may face an increased risk of conditions such as diabetes, congestive heart failure, and high blood pressure later in life.
The NHS emphasizes that while most cases of preeclampsia do not result in problems and often improve shortly after childbirth, there remains a possibility of severe complications.
These complications can affect both the mother and her baby, including the risk of eclampsia, a condition involving seizures that can be life-threatening for both mother and baby, although such cases are rare.
If you have preeclampsia, can you have a vaginal birth?
Women with preeclampsia can indeed have a vaginal birth, although the decision between a vaginal delivery and a cesarean section depends on various factors related to the health of both the mother and the baby.
According to an American Family Physician report, about 40% of women with preeclampsia are monitored for safe vaginal delivery, while the remainder may require a cesarean section.
This decision is based on the specific condition of the mother and the baby to choose the most suitable and safe delivery method.
While pregnant women with preeclampsia are often encouraged to opt for a cesarean section due to risks such as preterm birth and potential difficulties during labor, vaginal birth remains a possibility under certain conditions.
Particularly when the fetus has developed to 35 or 36 weeks, and the mother’s cervix is soft and prepared for delivery, natural birth can be a viable option.
In such cases, the doctor will have a detailed discussion with the pregnant woman and ensure close monitoring throughout the labor process.
This approach ensures that the delivery method is tailored to the best interests of both the mother and the baby, taking into account the specific circumstances of preeclampsia.
Does preeclampsia go away after delivery?
Yes, the signs and symptoms of preeclampsia most often go away after delivery, typically within 6 weeks.
The NICHD emphasizes this aspect, highlighting the importance of postpartum care for women who have experienced preeclampsia.
However, it’s important to note that the high blood pressure associated with preeclampsia can sometimes worsen during the first few days post-delivery.
Therefore, women who have had preeclampsia remain at risk for up to 6 weeks following the birth of their baby.
This period, known as postpartum preeclampsia, carries a higher risk of death, indicating the need for continued monitoring and care even after the baby is born.
What is postpartum preeclampsia?
Postpartum preeclampsia is an uncommon yet severe condition marked by elevated blood pressure and excessive protein in the urine, occurring after the baby’s birth.
Unlike preeclampsia, which usually arises during pregnancy and frequently improves after childbirth, postpartum preeclampsia occurs in the period following delivery.
According to Mayo Clinic , most cases of this condition develop within 48 hours of childbirth. However, it can also occur later, sometimes up to six weeks or more after childbirth, which is referred to as late postpartum preeclampsia.
The continuation or emergence of these symptoms in the postpartum period necessitates careful monitoring and prompt treatment.
If not addressed, postpartum preeclampsia can result in serious issues, including the occurrence of seizures.
The condition poses significant health risks and requires immediate medical intervention to prevent potentially life-threatening complications for the new mother.
Women and healthcare providers need to be aware of and responsive to any signs of preeclampsia that occur after delivery.
Will preeclampsia happen again in future pregnancies?
There is a possibility that preeclampsia can recur in future pregnancies, but the risk varies widely.
According to preeclampsia.org, the recurrence risk of preeclampsia in subsequent pregnancies ranges broadly from 13% to 65%.
This variation is influenced by several factors, including ethnicity, geographical region, and the Nature of clinical interventions in previous pregnancies.
A European Journal of Obstetrics & Gynecology and Reproductive Biology publication provides additional insights, stating that certain supplements or medications might reduce the likelihood of recurring preeclampsia.
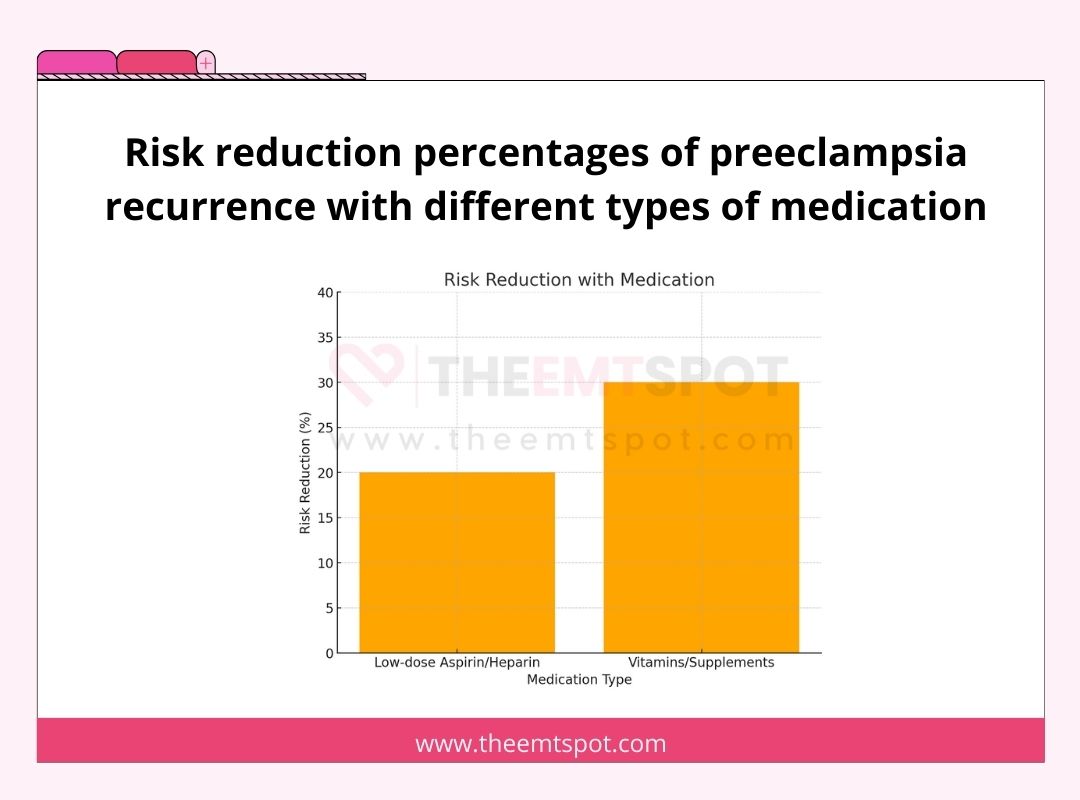
For instance, the use of low-dose aspirin or heparin has been shown to lower the risk of recurrent preeclampsia by 20% to 30%.
Vitamin D, omega-3s, calcium, and folic acid supplements may also decrease the risk.
Magnesium has also been found to reduce the risk of pregnancy-induced hypertension in some cases.
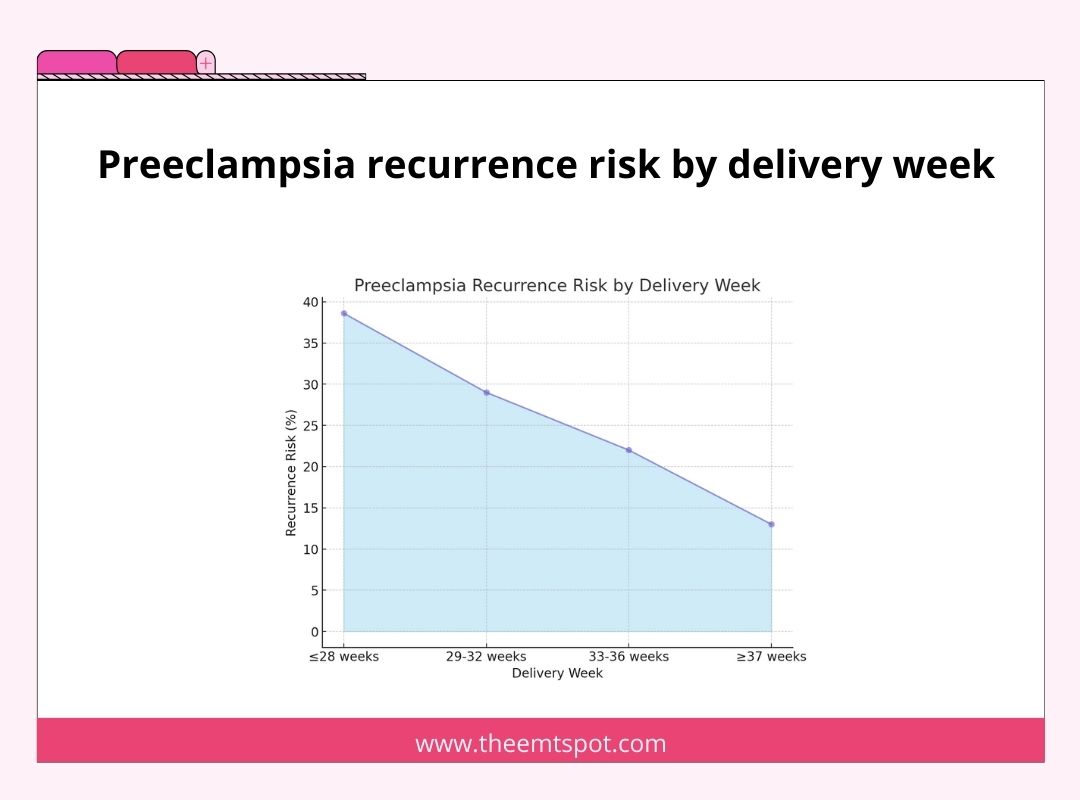
The timing of the first delivery also plays a role. The risk of preeclampsia recurring is higher (38.6%) if the first delivery occurred at or before 28 weeks of gestation.
This risk decreases with later deliveries. i.e., 29% for deliveries between 29-32 weeks, 22% for 33-36 weeks, and 13% for deliveries at 37 weeks or later.
The earlier preeclampsia occurs in a previous pregnancy, the greater the risk in subsequent pregnancies.
How to prevent preeclampsia during pregnancy?
Preventing preeclampsia during pregnancy involves adopting a range of health strategies, according to research reported by the Journal of Pregnancy.
Key among these is dietary management, particularly for women on low-calcium diets.
High-dose calcium supplementation has been identified as potentially beneficial in reducing the risk of preeclampsia.
Shireen Meher, a consultant in maternal-fetal medicine at Birmingham Women’s and Children’s NHS Foundation Trust, UK, highlights a review of clinical trials that demonstrated a reduction in preeclampsia risk by about 36% with high-dose mineral supplementation.
However, she notes the need for caution, stating:
“The quality of this data was considered relatively low because of significant variations in the underlying risk of preeclampsia in the women who participated in the trials, meaning that more evidence is needed.”
Meher explains the rationale behind this approach:
“It’s thought that low calcium might raise blood pressure by triggering the release of hormones like the parathyroid hormone and renin. Giving calcium supplements might reduce this hormone release and prevent blood vessel constricting, leading to hypertension.”
In addition to dietary adjustments, regular prenatal care is crucial for early detection and management of signs of preeclampsia.
Adopting a healthy lifestyle, including regular exercise, maintaining a healthy weight, and avoiding harmful substances such as tobacco and excessive alcohol, also plays a role in prevention.
Monitoring blood pressure regularly can aid in the early detection and management of hypertension, a key factor in preeclampsia.
Does aspirin really help to prevent preeclampsia?
Yes, aspirin does help in preventing preeclampsia. This is supported by both the U.S. Preventive Services Task Force (USPSTF) and the American College of Obstetricians and Gynecologists (ACOG), who recommend daily low-dose aspirin (81 mg) for women at high risk of developing preeclampsia.
Starting from the 12th week of pregnancy, there is a modest decrease in the likelihood of preeclampsia observed in high-risk women without causing adverse outcomes for the fetus, increasing maternal bleeding, or leading to placental issues.
This is especially beneficial for women with a history of preeclampsia, especially those who delivered preterm.
As explained below, aspirin is most suitable for specific groups of pregnant women.
- Those with chronic hypertension, renal disease, autoimmune diseases, type 1 or type 2 diabetes.
- Pregnant women carrying multiples (e.g., twins or triplets).
- Women with multiple risk factors for preeclampsia, such as it being their first pregnancy, older maternal age, a BMI over 30, a family history of preeclampsia, and certain sociodemographic characteristics.
Aspirin should be administered between the 12th and 28th weeks of gestation, preferably before 16 weeks, and continued daily until delivery.
The review by USPSTF found no significant difference in bleeding problems, such as maternal hemorrhage, fetal brain bleeding, or early separation of the placenta from the uterine wall, between the aspirin and placebo groups.
This suggests that the use of low-dose aspirin during pregnancy is safe and does not increase the risk of serious bleeding complications.
Why is it important to monitor blood pressure when you have preeclampsia?
Monitoring blood pressure is crucial when you have preeclampsia because it helps effectively manage and control the condition.
A 2023 study published in BMC Pregnancy and Childbirth by Atluri et al. reported that home-based monitoring improves patient outcomes and reduces risks for both the mother and the baby.
Regular monitoring allows for the early detection of any significant changes in blood pressure, which is vital for preventing severe complications associated with preeclampsia, such as stroke, organ damage, and eclampsia (seizures).
High blood pressure is a key indicator of the severity and progression of preeclampsia, and keeping it in check is essential for the health and safety of both the mother and the baby.
Women with preeclampsia can use home blood pressure monitors to monitor blood pressure at home.
These devices provide a convenient way to regularly check blood pressure levels without needing to visit a healthcare provider constantly.
It’s important to choose a reliable and clinically validated monitor and to follow the instructions carefully for accurate readings.
To maintain consistency, blood pressure should be recorded simultaneously each day, preferably in a seated position.
These readings can then be shared with healthcare providers during prenatal visits to assess the management plan for preeclampsia.
However, it’s essential to remember that home monitoring should not replace regular prenatal care, and any significant changes or concerns should be immediately communicated to a healthcare professional.
What blood pressure monitor should pregnant women buy?
Purchasing blood pressure monitor that offers a clinically valid result is the most crucial part of preeclampsia management.
The key to choosing the right monitor is to look for one that provides reliable readings.
When selecting the best blood pressure monitor, it’s crucial to consider several factors to ensure accurate and reliable readings, especially for specific populations such as seniors, pregnant women, or children.
Firstly, wrist and finger monitors are generally not recommended as they provide less reliable readings than upper arm monitors.
Choosing a monitor that has been clinically validated for accuracy is essential. If you’re uncertain about the validation of a monitor, consult a healthcare professional or pharmacist for guidance.
For specific populations like seniors, pregnant women, or children, ensure that the monitor is validated for these conditions, as their blood pressure monitoring needs can differ.
Lastly, the fit of the cuff is critical for accurate measurement. Measure the perimeter of your biceps and select a monitor with a cuff size that matches your measurement.
A properly fitting cuff is key to obtaining accurate readings and is a vital consideration in choosing the best blood pressure monitor.
Two of the most recommended models are the CheckMe BP2 and the Oxiline Pressure X Pro.
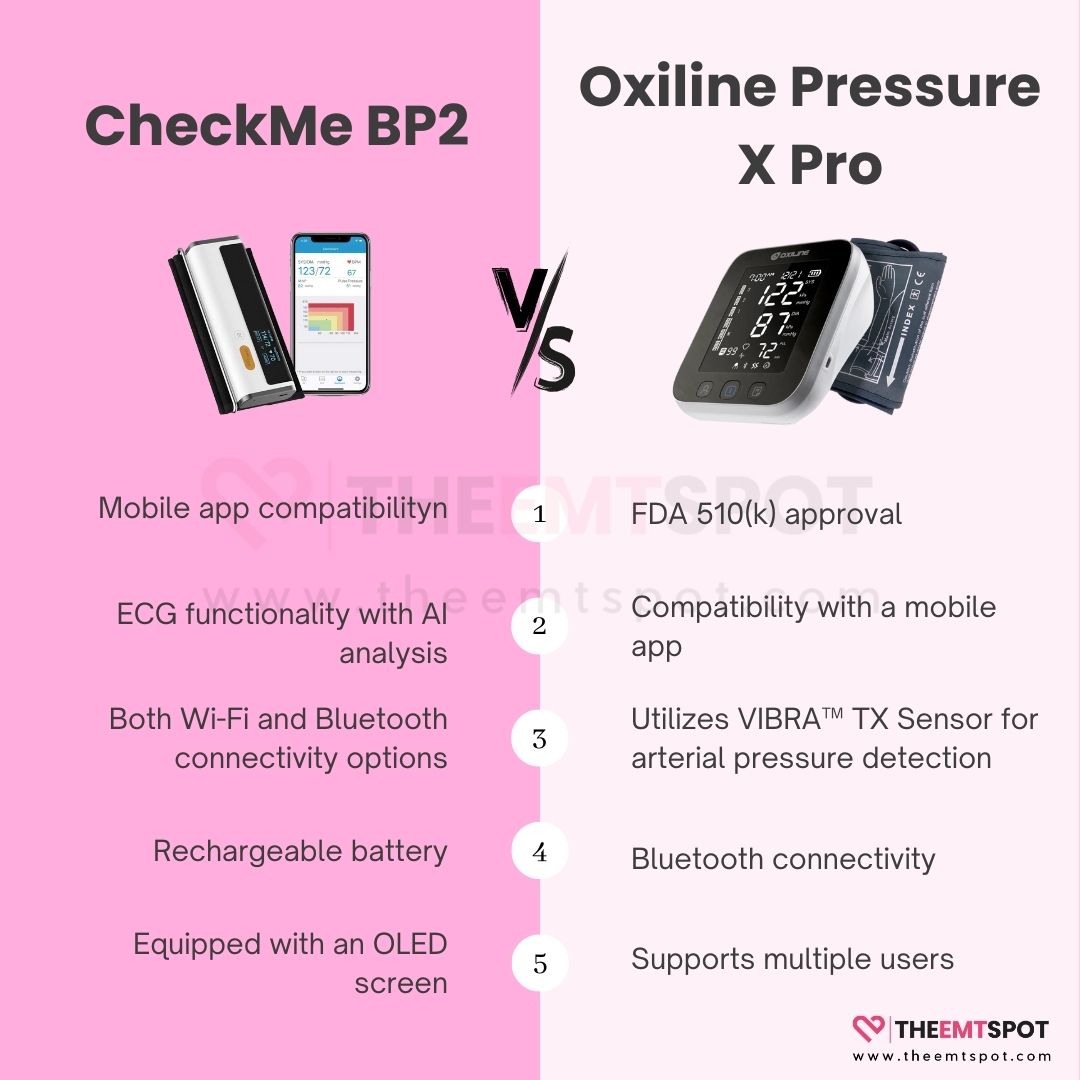
The first product is the Pressure X Pro from Oxiline, a well-known brand based in the United States, specifically Oxiline LLC. This device is highly impressive and boasts the following standout features.
- FDA 510(k) approval
- Compatibility with a mobile app
- Utilizes VIBRA™ TX Sensor for arterial pressure detection
- Bluetooth connectivity
- Backed by a lifetime warranty
- Supports multiple users
The second noteworthy product comes from CheckMe Care, a company based in Shenzhen, known for its exceptional app interface and data visualization capabilities. The CheckMe BP2 stands out from the rest with its impressive features, as highlighted below.
- Mobile app compatibility
- ECG functionality with AI analysis
- Both Wi-Fi and Bluetooth connectivity options
- Rechargeable battery
- Equipped with an OLED screen
- Real-time tracking capability
How to interpret a blood pressure chart for monitoring BP readings?
Interpreting a blood pressure chart is essential for monitoring blood pressure readings, especially for individuals managing conditions like preeclampsia.
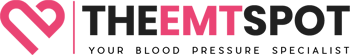
According to the Mayo Clinic, understanding blood pressure readings involves knowing the meanings of the systolic and diastolic numbers.
- Systolic Blood Pressure (Top Number): This measures the force the heart exerts on the walls of the arteries with each heartbeat.
- Diastolic Blood Pressure (Bottom Number): This measures the force the heart exerts on the walls of the arteries between beats.
The American College of Cardiology and the American Heart Association categorize blood pressure into four general categories:
- Normal Blood Pressure: Systolic below 120 mm Hg and Diastolic below 80 mm Hg. If your readings are here, maintain or adopt a healthy lifestyle.
- Elevated Blood Pressure: Systolic between 120-129 mm Hg and Diastolic below 80 mm Hg. In this case, you should also maintain or adopt a healthy lifestyle.
- Stage 1 High Blood Pressure (Hypertension): Systolic between 130-139 mm Hg or Diastolic between 80-89 mm Hg. Here, lifestyle changes are necessary, and you should talk to your provider about taking one or more medications.
- Stage 2 High Blood Pressure (Hypertension): Systolic 140 mm Hg or higher or Diastolic 90 mm Hg or higher. In this stage, adopting a healthy lifestyle and discussing the possibility of taking more than one medication with your provider is recommended.
A blood pressure measurement over 180/120 mm Hg is considered a hypertensive emergency or crisis and requires immediate medical attention.
For accurate blood pressure measurement, healthcare providers typically consider the average of two or more readings from three or more office visits. This average helps determine the appropriate treatment plan.
More in this topic






 Robin Backlund is a dedicated journalist and a medical student who has written several articles and essays exposing the falseness and hollowness of online resources in the medical science niche.
Robin Backlund is a dedicated journalist and a medical student who has written several articles and essays exposing the falseness and hollowness of online resources in the medical science niche.